HeLa Cells: Revolutionizing Research
Since their discovery in 1951, Hela cells, a strain of immortalized cells named after Henrietta Lacks, have been employed widely in scientific study. Henrietta Lacks, a 31-year-old African-American mother of five, was diagnosed with cervical cancer the same year she died. George Otto Gey, the director of the Tissue Culture Laboratory at the Johns Hopkins Hospital, collected and multiplied her cervical carcinoma cells, which proved exceptionally resilient and prolific, enabling their broad application in scientific research. In contrast to other human cells, HeLa cells could be maintained and multiplied in vitro, representing a considerable advance in medical research.
The History and Timeline of Hela Cells
Henrietta Lacks, a Black tobacco farmer, was taken to the Johns Hopkins Hospital in 1951 for abnormal vaginal bleeding and later received treatment for cervical cancer. Her first therapy consisted of taking tissue samples from her cervix without her consent. The cervical biopsy yielded tissue samples for George Otto Gey's clinical examination, which were studied in the tissue culture laboratory. In contrast to earlier specimens, Gey's lab assistant noted that the cells were doubling every 20–24 hours and expanding rapidly. Gey propagated the cervical cancer cells just before Lacks' death, and they were the first viable human in vitro cell line. The cells were named after the first two letters of Henrietta Lacks' first and last names and were given to any scientist who requested them to advance research.
Even though the cells were gathered without Lacks' or her family's permission, permission was neither necessary nor commonly requested at the time. There was no duty to warn patients or their family members that discarded or surgically obtained materials were the physician's or medical facility's property. In the 1970s, a public leak exposed Henrietta's actual name, and the Lacks family was asked for DNA samples to assist in identifying contaminated cell lines. The HeLa cell line originated from a sample of Lacks' cervical tissue and has been multiplied in cell culture to the extent that much exceeds the total number of cells in her body. There are several strains of HeLa cells as they continue to mutate in cell cultures, but all of them are the descendants of the tumor cells extracted from Lacks.
Addressing Historical Wrongs
The narrative surrounding Henrietta Lacks and the derivation of HeLa cells without her knowledge or consent has ignited a discourse on the ethics of medical research practices and the protection of individual rights, particularly concerning the use of human biological materials in science. Henrietta Lacks unknowingly became the source of the first immortal human cell line, which has since led to countless scientific breakthroughs. The realization of this ethical wrongdoing has catalyzed a shift towards more rigorous consent processes and a heightened awareness of the moral obligations of researchers. This case has not only highlighted the need for reform in research practices but also sparked a broader conversation about justice, respect, and recognition in medical research, leading to efforts to rectify past injustices and ensure that contributors to scientific advancement are acknowledged and treated with dignity.
Thermo Fisher and HeLa Cells
The lawsuit against biotech company Thermo Fisher Scientific related to HeLa cells was rooted in a deeper ethical and legal debate about the commercialization of biological materials derived from individuals without their consent. The case centered around the HeLa cell line, which led to significant scientific breakthroughs, including the development of the polio vaccine and advancements in cancer treatment.
The lawsuit brought to light several ethical considerations: the rights of individuals and their families over their biological materials, the historical context of taking samples from marginalized individuals without consent, and the responsibilities of companies benefiting from such materials. The case against Thermo Fisher Scientific highlighted the need for clearer policies and ethical standards regarding the use of human biological materials in research and commerce, ensuring respect for individuals' rights and equitable sharing of benefits arising from scientific discoveries.
For a detailed exploration of the origins, legal battles, and resolutions surrounding HeLa cells, check out our article "HeLa Cells: History, Lawsuit, and Settlements."
Fascinating Characteristics of HeLa Cells
HeLa cells are easy to culture and multiply rapidly and are also known for their high susceptibility to viral infections. They are particularly susceptible to human adenovirus 3, encephalomyocarditis virus, and poliovirus 1, 2, and 3. This characteristic makes HeLa cells essential for studying these viruses' replication, assembly, and pathogenesis and developing new antiviral strategies. In addition, HeLa cells are widely used as transfection hosts for studying gene function and regulation, recombinant protein production, and gene therapy.
- Even for cancer cells, HeLa cells have an abnormally high rate of cell proliferation and limitless lifespan, making them excellent for scientific inquiry.
- HeLa cells have an active telomerase form, enabling limitless cell division and immortality.
- HeLa cells overcome the Hayflick limit, the maximum number of cell divisions most normal cells may undergo before becoming senescent.
- HeLa cells have a hypertriploid chromosomal number (3n+). The average chromosome number in HeLa cells is 82 but can range from 70 to 164 (rather than the standard diploid number of 46). These chromosomes are referred to as "HeLa signature chromosomes.". Hela cells have a complex karyotype characterized by a high degree of aneuploidy and structural rearrangements. HeLa cells have a small telocentric chromosome in 98% of cells and 100% aneuploidy in 1385 cells examined. These chromosomal abnormalities play an essential role in the rapid growth rate and immortality of HeLa cells and are also associated with cervical cancer.
- Due to horizontal gene transfer from human papillomavirus 18 (HPV18) to human cervical cells, HeLa cells have a different genome from Henrietta Lacks.
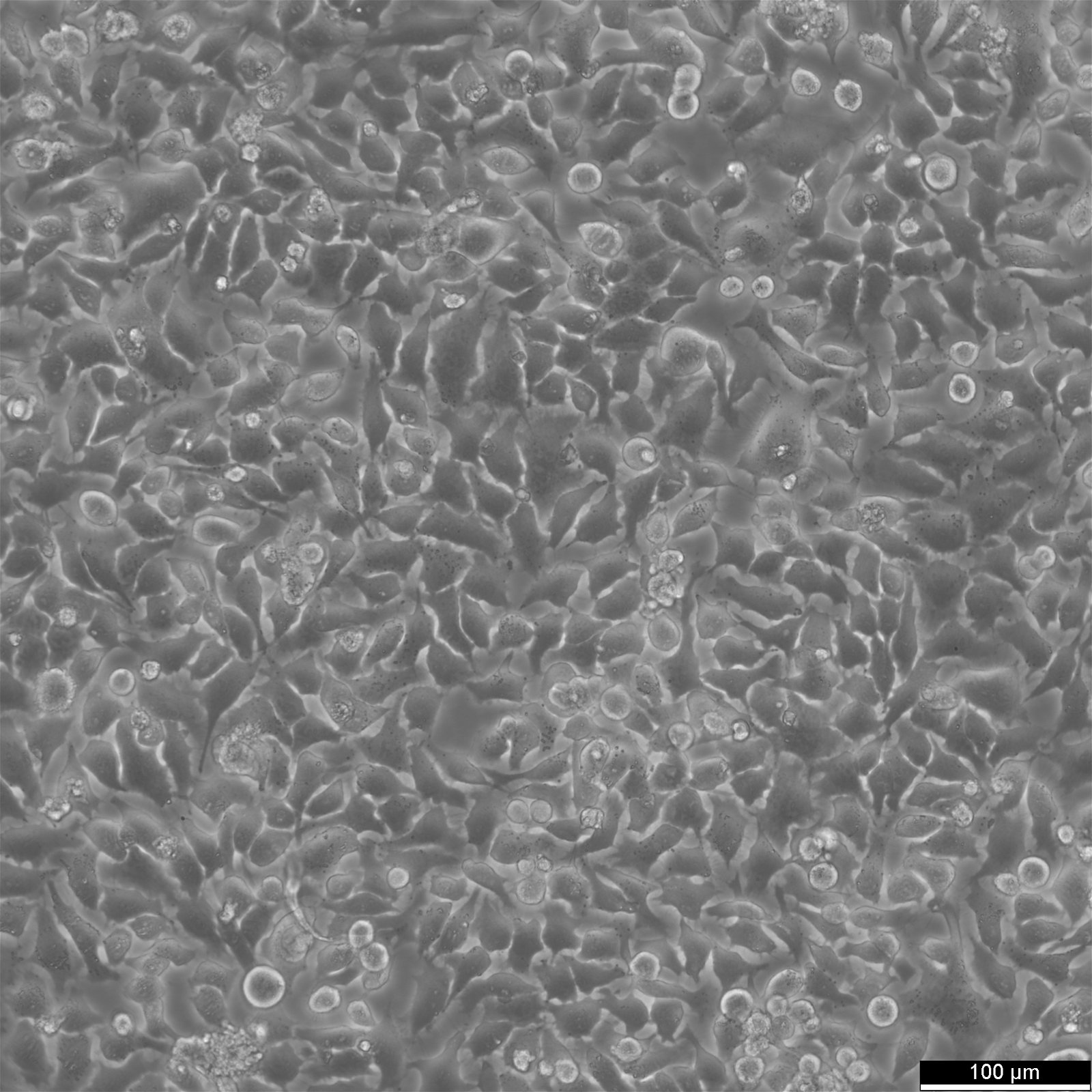
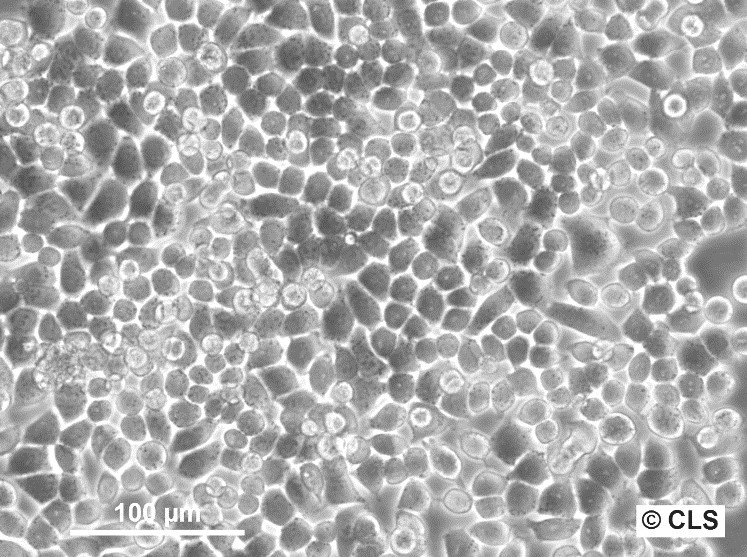
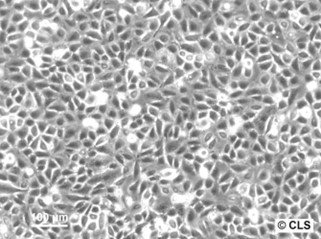
Structure of HeLa Cells
HeLa cells have a diameter of 10 - 20 µm, depending on culture conditions. Most mammalian cells have a diameter between 10 and 100 µm. One of the smallest human cells, red blood cells, have a diameter of about 8 µm. On the other hand, muscle fiber cells and neurons can be extremely long.
Research Advances Thanks to HeLa
HeLa cells have been at the heart of significant research advances, including discoveries in genetics, virology, and therapeutic development. The HeLa cell line has been used to study cancer, AIDS, the effects of radiation and toxins, gene mapping, and countless other scientific endeavors. Over 60,000 scientific articles have been published on HeLa research, increasing by more than 300 monthly.
Polio eradication
In the 1950s, Jonas Salk tested the first polio vaccine using HeLa cells. These cells were susceptible to poliomyelitis infection, resulting in the death of infected cells. As a result, HeLa cells were in high demand for polio vaccine testing because results were readily available.
Virology
HeLa cells have been infected with numerous viruses, including HIV, Zika, herpes, and mumps, to test and develop new vaccines and drugs. Dr. Richard Axel discovered that HeLa cells can be infected with HIV by adding the CD4 protein so that the virus can be studied. HeLa cells have been used to research papillomavirus E2 expression and apoptosis, and they have also played an essential role in the development of human papillomavirus (HPV) vaccines.
Cancer
HeLa cells have been used for numerous cancer studies, including sex steroid hormones such as estradiol, estrogen, and estrogen receptors and estrogen-like compounds such as quercetin and its cancer-preventive properties. HeLa cells have also been used to study the effects of flavonoids and antioxidants with estradiol on cancer cell proliferation.
Other noteworthy applications include
- Cancer treatments: Hela cells were crucial in creating cancer medicines, such as camptothecin, an FDA-approved pharmaceutical for treating ovarian, lung, and cervical cancer.
- Thalidomide and Multiple Myeloma: HeLa cells were used to illustrate how the medication thalidomide, which was initially used for morning sickness, may cause congenital disabilities, leading to its usage in the treatment of multiple myeloma.
- Understanding HIV and AIDS: The revelation that HIV had difficulties infecting HeLa cells improved researchers' understanding of the virus, opening the door for developing HIV and AIDS medications.
- Cellular Aging: HeLa cells have enabled researchers to explore the biology of aging and the diseases that cause premature aging, leading to the discovery of regenerable chromosomes that prevent cellular degeneration and damage over time.
- Blood Disorders: HeLa cells were used to evaluate the efficiency of hydroxyurea against different blood malignancies and anemia; hydroxyurea is now used to treat sickle cell disease and white blood cell malignancies.
- X-rays: In 1956, scientists utilized HeLa cells to investigate the effects of X-ray radiation on live organisms, gaining a better understanding of the hazards of high and recurrent doses of radiation from medical X-rays.
- Innovative Discoveries: HeLa cells have played a crucial part in several significant discoveries in biology, leading to advances in cancer medicines, knowledge of HIV/AIDS, and more.
- Cellular aging: Researchers employing HeLa cells were awarded the Nobel Prize for their findings about cellular aging and preventing cellular degeneration and damage over time.
Explore HeLa cells and their derivatives
What are potentially immortalized cells?
Immortalized cell lines are cells that have been modified so that they divide continuously and can be grown over long periods. They come from sources with chromosomal abnormalities or mutations and can be derived from tumors. To continue growth, scientists divide some of the cells into new cell culture vessels and multiply them for further experiments.
HeLa cells, like other cell lines, are considered "immortal" because they can divide indefinitely in cell culture flasks as long as the primary conditions for cell survival are maintained (i.e., supported and cared for in an appropriate environment). There are numerous strains of HeLa cells because they keep mutating in cell cultures, but they all derive from the same Lacks tumor cells. The number of HeLa cells propagated in cell cultures far exceeds that found in Henrietta Lacks' body.
HeLa Cell Manufacturing, Quality Control, and Shelf life
HeLa cells may be cultivated and harvested using standard cell culture methods at around 80–90% confluence. The cells are relatively simple to manipulate and may be cultured in various settings.
How to defrost frozen HeLa cells
- Put the cryovial in an antibacterial 37°C water bath with clean water.
- Rapidly thaw for 40 to 60 seconds. The vial should be removed and transferred to a sterile flow cabinet.
- Wipe the vial with 70% alcohol and transfer the cell suspension into a 15 ml centrifuge tube containing 8 ml of culture medium.
- Reconstitute the cells, centrifuge at 300 x g for three minutes, and discard the supernatant (alternatively, dilute with medium and remove the freezing medium 24 hours later if not centrifuging straight away).
- Transfer the cells suspended in 10 ml of new culture media to two T25 cell culture flasks.
Subculturing HeLa cells
- Remove the old medium from the cell culture flask.
- Rinse the adherent cells using PBS without calcium and magnesium. Use 3-5 ml of PBS for T25, and 5-10 ml for T75 cell culture flasks.
- Add Accutase to the cell culture flask. Use 1-2 ml per T25, and 2.5 ml per T75 cell culture flask. Ensure that the cell sheet is completely covered.
- Incubate the cell culture flask at ambient temperature for 8-10 minutes.
- Carefully resuspend the cells with the medium. Add 10 ml of medium and gently pipette up and down to break up cell aggregates.
- Centrifuge the cell suspension for 3 minutes at 300 x g.
- Resuspend the cells in fresh medium.
- Dispense the resuspended cells into new cell culture flasks that contain fresh medium.
- Store the cells in liquid nitrogen for long-term storage.
By following these steps, you can subculture cells and maintain a healthy cell culture for future experiments.